Across Africa, many women are told their severe period pain is “normal” or “that is just part of being a woman.” But for those living with endometriosis, the pain goes far beyond cramps.
The chronic pelvic pain associated with endometriosis can affect your education, career, intimacy, fertility, and emotional wellbeing, long before a diagnosis is made.
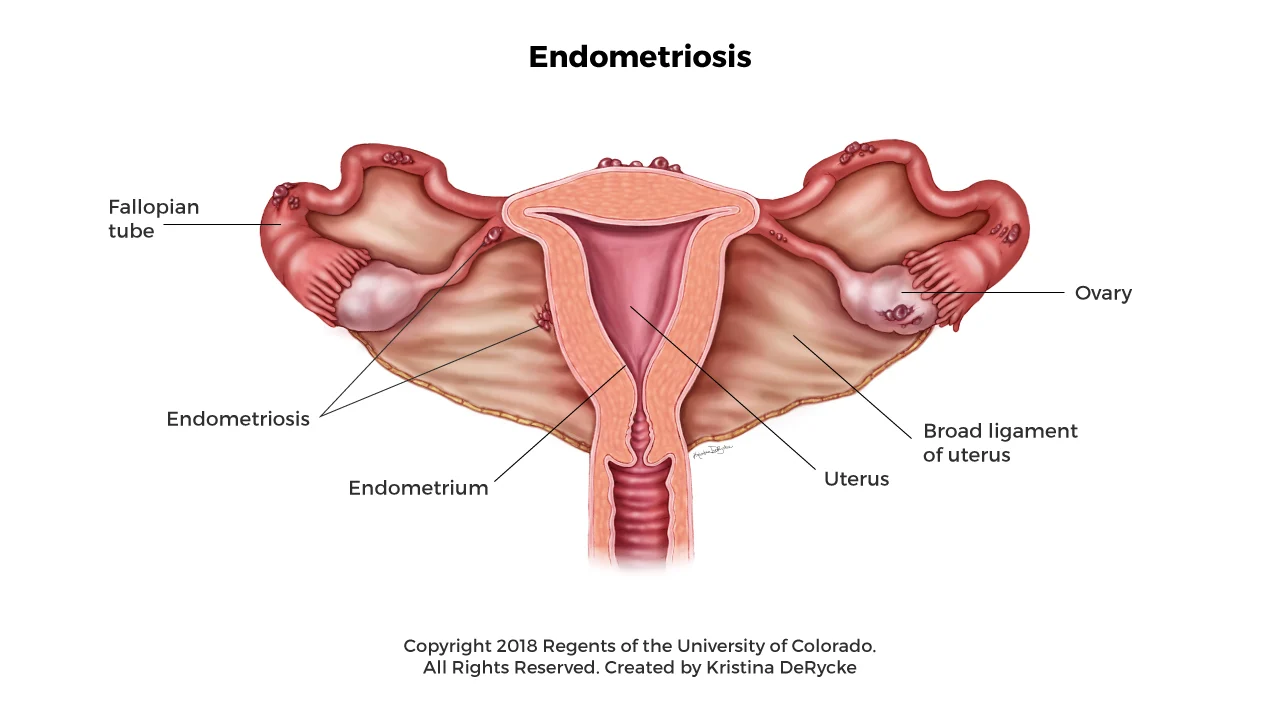
What Is Endometriosis?
Endometriosis is a condition where tissue similar to the lining of the womb grows in places it shouldn’t. Instead of staying inside the uterus, it can grow on the:
- ovaries
- fallopian tubes
- outer wall of the uterus
- pelvic lining
- bowel
- bladder
- diaphragm or chest (in rare cases)
This tissue responds to your menstrual cycle hormones, mainly estrogen and progesterone in the same way the uterine lining does.
During each cycle, it thickens, breaks down, and bleeds, but because it’s outside the womb, the blood has nowhere to go.
Over time, this trapped bleeding leads to:
- swelling and inflammation
- scar tissue
- organs sticking together (adhesions)
- chronic pelvic and back pain
Some people have intense symptoms. Others have mild or no pain at all but still experience complications like infertility.
Endometriosis often begins in the teenage years or early adulthood, but many people aren’t diagnosed until their 30s or 40s.
What Causes Endometriosis?
The exact cause of endometriosis isn’t fully understood, but experts believe several factors may play a role. For some people, genetics are involved, which is why the condition can appear across generations.
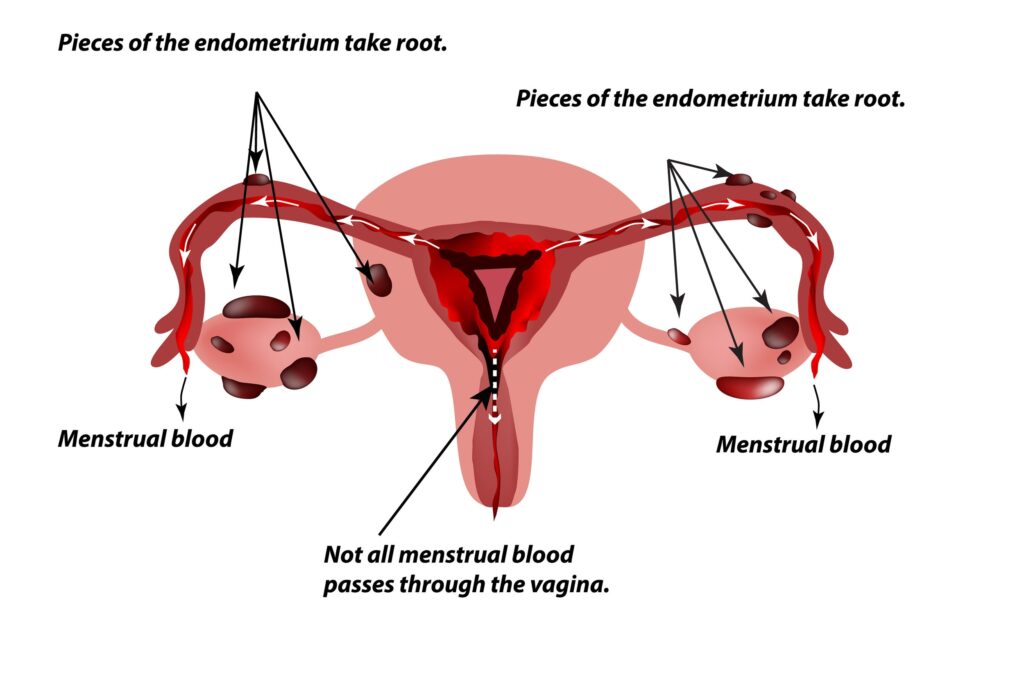
There’s also the theory of retrograde menstruation, where menstrual blood flows backward into the pelvis, allowing tissue to settle where it shouldn’t. Changes in the immune system may also make it harder for the body to clear this misplaced tissue.
Hormones, especially higher estrogen levels, can intensify symptoms, and environmental or inflammatory factors may influence how the disease progresses. Together, these factors help explain why endometriosis looks so different from one person to another.
How to Know If It’s Endometriosis or ‘Normal’ Period Pain
Normal period cramps are uncomfortable but usually:
- improve with simple pain medications
- last 1–3 days
- don’t disrupt your day-to-day life
With endometriosis, the pain is usually deeper, lasts longer, and affects your day-to-day life.
Early warning signs
These early symptoms often get ignored or normalised:
- cramps so severe you can’t walk, work, or attend school
- pain that worsens over time instead of improving
- heavy bleeding or bleeding between periods
- pelvic or lower back pain before, during, or after your period
- pain during or after sex (dyspareunia)
- fatigue that feels out of proportion to your activity
- bloating around your period (“endo belly”)
If your period pain regularly stops you from functioning, it’s not “just cramps.” Consider talking with a healthcare professional for a proper diagnosis.
Less obvious symptoms
Endometriosis can also affect the bowel, bladder, and in rare cases, areas like the diaphragm or chest.
You may notice:
- diarrhea
- constipation
- painful bowel movements
- stomach cramps that worsen during periods
- pain when urinating or needing to pee often
- blood in stool or urine during menstruation
- shoulder pain during your period (from diaphragm involvement)
- chest pain or trouble breathing around your period (rare)
These symptoms are often easy to treat one by one, like ‘just a stomach issue’ or ‘just an infection,’ without realizing they might be part of endometriosis.
Silent endometriosis
Some people have endometriosis with almost no cramps at all. Instead, they may struggle with:
- infertility
- ovarian cysts
- severe internal scarring
- incidental diagnosis during surgery for another issue
This is sometimes called silent endometriosis. The disease may still be progressing, but because the pain isn’t always extreme, it often gets missed or dismissed.
Why Endometriosis Is Often Missed in Africa
Across the continent, many women grow up believing that painful periods are “normal,” “a sign of strength,” or simply “what women are expected to handle.”
So many women end up pushing through the pain with over-the-counter pain medications, and silence, without realizing that this very endurance is what delays diagnosis.
Diagnosis is also harder because of several systemic and cultural barriers:
- Stigma around menstrual and sexual health: Many girls are taught not to talk about periods, pain, or “private parts,” so they hide symptoms until they become unbearable.
- Low awareness among the public and some healthcare professionals: Many women don’t know endometriosis exists, and some clinicians dismiss symptoms as “normal cramps” or “hormonal changes,” leading to repeated misdiagnosis.
- Limited access to gynecologists and laparoscopy in public hospitals: Most public facilities lack specialists and advanced imaging, meaning many women only get a diagnosis after years of untreated pain or infertility.
- Cultural expectations to endure pain quietly: In many homes, girls are praised for “being strong,” so even severe pain is normalized, and asking for help can be viewed as weakness or exaggeration.
Research shows that globally, a diagnosis can take 7–10 years, and this delay is often longer in African settings where symptoms are easily dismissed or misunderstood.
How Endometriosis Affects Daily Life
Endometriosis doesn’t just affect the body. Studies show it can influence how you work, study, relate to others, and feel about yourself.
For many African girls and women, this looks like:
- Missing school every month, getting labeled as “lazy” or “unserious” when you were actually too sick to go.
- Having trouble performing well at work due to flare ups, and being judged by others as untrustworthy or overly dramatic.
- Cooking, cleaning, or caring for family while in pain, often without rest and with no recognition of how heavy that burden is.
- Avoiding intimacy with your partner, due to the fact that sex hurts, and causing a lack of understanding from them.
- Living with chronic fatigue or physical exhaustion, for many years after being told “this is all in your head” or “you’re just making it up”.
Stages of Endometriosis
Doctors classify endometriosis into four stages based on how much tissue is present, how deep it grows, and whether cysts or scar tissue are involved.
Stage I: Minimal
A few small, shallow lesions with little to no scar tissue.
Stage II: Mild
More lesions than stage I, and they may grow a bit deeper into surrounding tissue.
Stage III: Moderate
Deep implants are present along with small ovarian cysts (endometriomas) and noticeable scar tissue.
Stage IV: Severe
Large cysts, extensive deep lesions, and dense adhesions that can cause organs to stick together.
However, the stage doesn’t always match how someone feels. A person with stage I may have disabling pain, while another with stage IV may have very mild symptoms.
How Endometriosis Is Diagnosed
There is no single blood test for endometriosis. Diagnosis usually involves:
- History and physical exam: A doctor will ask about your pain, periods, sex life, bowel habits, and family history. They may gently press your abdomen or do a pelvic exam to check for tender areas, swelling, or cysts.
- Pelvic ultrasound: A painless scan that uses sound waves to look at your uterus and ovaries. It can detect ovarian cysts but may miss small endometriosis lesions.
- MRI scan: A detailed imaging test that shows deeper lesions and organs clearly. It’s helpful for complex cases but expensive and not widely available in many regions.
- Laparoscopy: A minor surgical procedure where a small cut is made near the belly button and a camera is inserted to look directly at the organs. Doctors can confirm endometriosis and sometimes treat it during the same procedure.
In many African countries, laparoscopy is available mainly in private or referral hospitals, which makes early diagnosis harder for many women.
Treatment Options in Africa
Endometriosis has no permanent cure yet, but doctors can manage symptoms through medical care, lifestyle adjustments, and supportive strategies.
Pain relief and hormonal treatment
Common options include:
- NSAIDs such as ibuprofen or diclofenac
- combined birth control pills
- progestin-only methods (pills, injections, hormonal IUDs)
- GnRH agonists for severe cases
Surgical options
If medication isn’t enough, doctors may recommend laparoscopic surgery to remove or burn endometriosis lesions, release adhesions, and remove ovarian cysts.
Surgery can improve pain and fertility, but:
- symptoms can return
- costs may be high without insurance
- there is a shortage of trained endometriosis surgeons in many African regions
Supportive and lifestyle approaches
These don’t cure endometriosis, but they may help reduce flare-ups:
- gentle movement, like walking, stretching, or yoga
- stress-management practices, such as breathing exercises, meditation, or journaling
- anti-inflammatory diet, focusing on whole foods, fruits, vegetables, lean proteins, and omega-3 sources
- herbal remedies used with professional guidance, for example research shows that ginger may help ease menstrual pain
Always speak with a healthcare professional before combining herbs with hormonal medication to avoid potential interactions.
Frequently Asked Questions
Can endometriosis be cured?
There is no cure yet. Surgery and hormonal treatments can reduce or remove visible disease and relieve symptoms, but endometriosis can return.
How painful is endometriosis really?
Pain ranges from mild to completely disabling. It can feel like sharp stabbing, pulling, burning, or deep aching that doesn’t respond well to pain medications.
Is endometriosis common in African women?
Yes. Research suggests it is likely as common as in other regions, but many cases remain undiagnosed due to stigma, low awareness, and limited access to specialized care.
Conclusion
Endometriosis is a complex medical condition that affects your health, relationships, and your quality of life. For too long, severe menstrual pain has been dismissed as something women should simply endure, especially in African communities.
Recognizing symptoms early, seeking care, and understanding your treatment options can help you get the support you deserve. The more we talk about endometriosis, the more we reduce the silence and stigma surrounding it.