In Nigeria, hirsutism is sometimes unfairly framed as an “Igbo women’s problem,” a stereotype that distracts from the real medical causes. Online forums often fuel these myths, linking excess hair growth to ethnicity or “good genes.” But in reality, hirsutism is a medical condition with biological explanations, not cultural ones.
What Hirsutism Really Is
Hirsutism (pronounced HUR-soot-iz-um) is a medical condition in women that causes excessive growth of coarse, dark hair in areas where men typically grow hair such as the chin, chest, stomach, or back.

What Causes Hirsutism?
Hirsutism happens when the body produces too much of the male hormone called androgens. Women naturally produce androgens, but usually in small amounts. When levels rise above normal, it can trigger excess hair growth as well as other changes, such as acne, voice deepening, or differences in body shape.
In some cases, hormone levels look normal, but the hair follicles are extra sensitive to androgens. This sensitivity alone can cause thick, dark hair to grow in areas where women typically do not have it.
Some common reasons for higher androgen activity include:
Polycystic Ovary Syndrome (PCOS): A hormonal condition that often leads to small cysts on the ovaries and disrupts the balance of estrogen and androgens.
Cushing’s Syndrome: Caused by long-term exposure to high levels of cortisol, the body’s main stress hormone.
Hormone-producing tumors: Rare growths in the ovaries or adrenal glands that increase androgen production.
Certain medications: Drugs like anabolic steroids, treatments that encourage hair growth (such as minoxidil), or danazol (used for endometriosis) can lead to unwanted facial or body hair.
High insulin levels: When insulin is too high, it can push the ovaries to release more androgens.
Congenital adrenal hyperplasia: An inherited condition that affects how the adrenal glands make hormones, sometimes leading to excess androgen.
Menopause: Hormonal shifts after menopause may cause new or increased facial and body hair.
Idiopathic causes: Sometimes, no medical explanation is found.
PCOS VS Hirsutism
Polycystic Ovary Syndrome (PCOS) is one of the most common causes of hirsutism, but they are not the same condition. Women with PCOS often have additional symptoms like irregular periods, acne, weight changes, or fertility struggles. Hirsutism, on its own, may appear without any other PCOS signs.
Diagnosing Hirsutism
Doctors usually begin with a physical exam, checking hair growth patterns and related symptoms. To understand the root cause, they may recommend:
- Blood work to measure hormone levels.
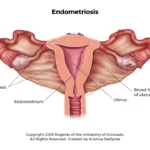
- Ultrasound scans to check the ovaries and uterus for cysts or irregularities.
- CT scans or X-rays of the adrenal glands to rule out abnormalities.
- MRI scans if a problem in the brain or pituitary gland is suspected.
- Pelvic examination to look for ovarian cysts or tumors.
They may also use the Ferriman–Gallwey scale, which scores hair growth across nine body areas from 0 to 4. A higher total score signals more severe hirsutism.
Treating Hirsutism
Treatment depends on the cause, severity, and personal preference. Options include:
Lifestyle and self-care
- Weight management: Losing weight can lower androgen levels.
- Shaving, tweezing, waxing, or threading: Common but temporary methods of hair removal.
- Depilatory creams: Break down hair chemically (patch test recommended).
- Bleaching: Lightens hair to make it less visible.
Medical and long-term options
- Laser hair removal: Uses heat to damage follicles; may require multiple sessions.
- Electrolysis: Permanently destroys hair follicles using electric current.
- Medications:
In some cases, doctors may prescribe medications to help manage symptoms or address hormone imbalances. The specific choice depends on the individual’s diagnosis, and only a healthcare provider can determine what’s safe and effective.
Hair growth patterns are complex, medical, and individual. They are not tied to tribe, culture, or stereotypes. If you notice unusual or distressing hair growth, the best step is to see a qualified doctor who can identify the underlying cause and guide you toward safe, effective care.
Frequently Asked Questions (FAQ) About Hirsutism
Is hirsutism the same as just being hairy?
No. Many women naturally have body hair. Hirsutism refers specifically to coarse, dark hair growing in areas where women don’t usually grow much hair, like the chin, chest, or back.
Can hirsutism affect any woman?
Yes. Hirsutism can affect women of any tribe, race, or background. It’s not linked to ethnicity or culture—it’s a medical condition.
Is hirsutism always caused by PCOS?
Not always. PCOS is a common cause, but hirsutism can also be linked to hormonal imbalances, certain medications, menopause, or even run in families without an obvious medical cause.
Can hirsutism go away on its own?
Sometimes mild cases improve with lifestyle changes, like weight management. But often, a medical evaluation is needed to find and treat the root cause.
Does hirsutism mean I can’t get pregnant?
Not necessarily. While conditions like PCOS can affect fertility, hirsutism itself does not automatically mean infertility. Many women with hirsutism conceive and have healthy pregnancies.
Should I see a doctor about hirsutism?
Yes, especially if the hair growth is sudden, severe, or accompanied by other symptoms like irregular periods, acne, or voice changes. A doctor can check for underlying health conditions and recommend safe treatment options.